Relevance of the topic. In today's world, it is difficult to find women who are not familiar with the problem of premenstrual syndrome (PMS). Premenstrual syndrome is the cyclical appearance of a complex of various symptoms and psychoemotional disorders that occur 2-10 days before menstruation and disrupt the woman's usual way of life. Severe forms of PMS are observed in 3-8% of women of reproductive age. At least 20% of the symptoms of PMS are such that require a drug therapy administration. Many different factors: stress, gynecological diseases, infections, metabolic disorders, lack of physical activity, intellectual work affect the contraction of PMS. There is higher incidence among the representatives of the Caucasoid race, residents of large cities [1-3].
Causative factors: disruption of the ratio of estrogen to progesterone;; relative increase of prolactin in the blood, which contributes to the sodium-retarding effect of aldosterone and antidiuretic action of vasopressin and changes in the functioning of the renin-angiotensin-aldosterone system (increased fluid in the body); monthly cyclic fluctuations in the number of certain neurotransmitters in the brain, including endorphins, serotonin, prostaglandins, which lead to increased pain impulses; hyponutrition: a deficiency of vitamin B6 (breast sensitivity, fatigue), magnesium deficiency (chocolate craving, tachycardia); hereditary factor: identical twins are much more likely to suffer PMS together than non-identical. (so-called "genetic predisposition").
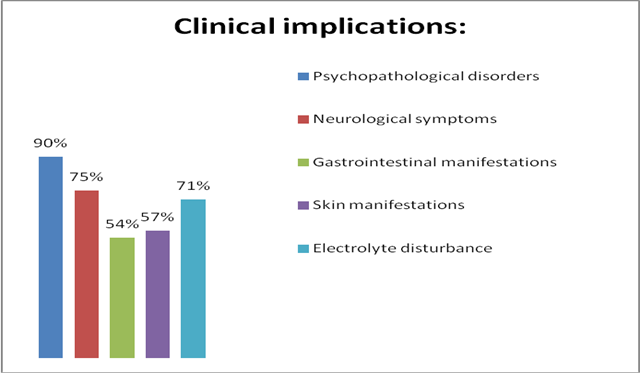
Clinical implications of PMS are very diverse and vivid. Physical signs: 1) Psychopathological disorders (emotional instability, irritability, agitation, depression, tearfulness, apathy, memory impairment, fatigue, atony, sleep disturbance, suicidal thoughts, disorder of libido, sense of fear, smells or sounds hypersensitivity); 2) Neurological symptoms (headache, dizziness, incoordination, hyperesthesia, pain in the heart, arrhythmia); 3) Electrolyte disturbance (peripheral edema, weight gain, pain in the mammary glands, bloating, disorder of diuresis); 4) Gastrointestinal manifestations (changes in appetite and taste preferences, nausea, vomiting, flatulency); 5) Skin manifestations (acne vulgaris, skin oiliness change, increased sweating, hives, itching, hyperpigmentation); 6) Cryptic manifestations (attacks on the type of sympathoadrenal crises occurring before menstruation); 7) Musculoskeletal manifestations (pain in the bones, muscles, joints; decrease in muscle strength) [4-5].
Since the symptoms are very nonspecific, for the diagnosis of PMS, a competent medical consultation is needed. Age is not significant, any woman in the period from menarche to menopause can experience the symptoms of PMS. Most commonly the disease onsets to 25-30 years [3]. In today's world, gaining popularity menstrual symptoms calendars and visual analogue scale (VAS) allow to determine not only the presence of specific symptoms of PMS, but also its severity and duration. Various studies, in particular ultrasonography of the pelvic organs are made to clarify the nature of the menstrual cycle (with PMS usually ovulatory) and the elimination of concomitant gynecological pathology, ultrasonography of the mammary glands before and after menstruation for differential diagnosis with fibroadenomatosis of the mammary glands, hormonal studies to assess the level of estrogen, progesterone, follicle-stimulating hormone, prolactin, luteinizing hormone, testosterone, adrenal hormones and others. In detecting hyperprolactinemia, the identification of triiodothyronine, thyroxine and thyrotropin (TTH) in the blood serum makes it possible to exclude primary hypothyroidism. With prolactinemia above 1000 mIU / l, an MRI of the hypothalamo-pituitary region is performed to detect prolactinoma. In the form of a crisis that proceeds with an increase in arterial blood pressure, differential diagnosis with pheochromocytoma (identification of catecholamines in after the attacks urine, adrenal MRI) is necessary. However, in many cases when listed sudies are insufficient, additional methods are used: electrocardiography, electroencephalography, brain MRI, ultrasonography of the thyroid gland, mammography, full blood count and urine analysis to exclude violations from other systems and organs.
By now, various therapeutic interventions have been proposed, aimed at alleviating premenstrual symptoms. The key to successful treatment of any disease is a multifaceted approach [6-7]. In the treatment of premenstrual syndrome, it is important to combine a healthy lifestyle, proper nutrition, treatment of comorbidity, physiotherapy procedures. For pharmacological therapy of premenstrual syndrome, various medications that can be divided into two large groups are used:
1. Hormonal preparations are prescribed only after a thorough examination of the hormonal background. Combined oral contraceptives (more often than not, monophasic preparations that contain 21 tablets with the same content of estrogens and progestins) and oral progestogens are used. Other regulators of the level of hormones in the blood are used too, for example, blockers of prolactin production (cabergoline, bromocriptine). Of non-hormonal drugs that affect the production of hormones, buserelin and tryptorelin are also used (they stimulate the production of sex hormones). On the hormonal balance can affect herbal remedies.
2/ Non-hormonal preparations is a large group of drugs used to treat premenstrual syndrome. In this group we can distinguish:
- Medicines that improve the blood supply of tissues (pentoxifylline, nicergoline).
- Preparations that stimulate metabolic processes. These include vitamins and minerals in various combinations, biogenic stimulants (erbisol, coenzyme Q10).
- Non-steroidal anti-inflammatory drugs that are used in severe pain syndrome and fluid retention in the body (diclofenac, indomethacin). They reduce the formation of prostaglandins.
- Diuretics (spironolactone).
- With florid psychoneurological symptoms serotonergic drugs (zolmitriptan - for the treatment of migraine attacks); histaminergic (betagistin - for symptomatic treatment of dizziness); "major" and "minor" tranquilizers are used. Also, nootropic drugs, such as pyracetam stimulating the function of the nervous system are used.
- Recently, in the treatment of premenstrual syndrome, an important role is played by botanical medicines, because plant extracts are better tolerated, suitable for long-term treatment and at the same time have sufficient effectiveness.
Materials, methods and results of the study. An anonymous survey of 250 female students of the Kharkiv National University at the age of 19-22 was conducted. After analyzing the results of the questionnaires, we determined that the most common clinical manifestations are emotional instability, apathy, arousal and tearfulness, which are related to psychopathological disorders. However, many girls noted the appearance of headache, tenderness of the mammary glands, peripheral edema, a change of skin oiliness and an increase in body weight. In addition, the severity of the symptoms of the menstrual cycle depends on the individual characteristics of the body and the presence of diseases. If there are problems with the gastrointestinal tract, then before the onset of PMS, there will be a pain in the stomach, an intestinal disorder. In the case of the sensitive nervous system, it will be the first system which suffers during the PMS period. That is why the question about drug correction arises:

According to the questionnaire, , girls think of the use of medicines only when there are strong and intolerable violations from any system. However, it should be noted that only 5% of women with severe PMS require the drug treatment of premenstrual syndrome.
As known, manifestations of premenstrual syndrome are associated with cyclic hormonal changes in the female body. Therefore, hormonal therapy of pathology is carried out through various effects on the level of sex hormones. In 4% of cases the girls took hormonal preparations, namely: Utrozhestan (micronized progesterone), Danazol (representative of antigonadotropins), Zoladex (antagonist of gonadotropin-releasing factor) and various COCs basis of which is to suppress ovulation, which in theory should help to eliminate premenstrual syndrome.
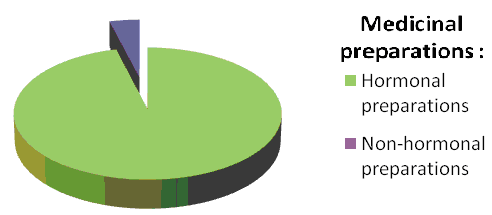
In the remaining 96% of cases, the girls used non-hormonal drugs. Their spectrum of action is very wide. The choice of the drug depended on the symptoms that arose. With edematous forms and with a cephalgic variant of the syndrome, accompanied by an increase in intracranial pressure, the girls used diuretics, for example, Spironolactone (Veroshpiron) (K-saving diuretic, Aldosteron antagonist).
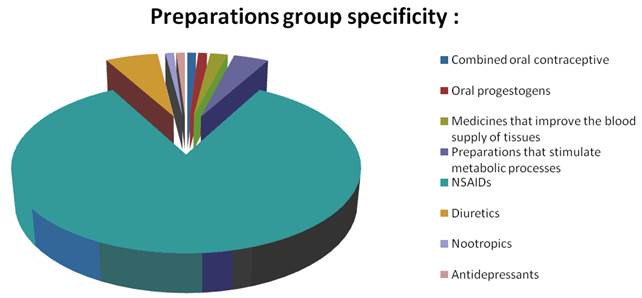
Antidepressants reduce symptoms, if the psychoemotional component predominates among the symptoms of the pathological state (depression, irritability, emotional instability, etc.). Among antidepressants, Cipramil, Fluoxetine and Sertraline are the most effective (according to questionnaires).
However, the most common preparations are NSAIDs: Ibuprofen (a derivative of propionic acid), Ketorolac (a derivative of pirolizinkarbonovoy acid), ketoprofen (a derivative of propionic acid), indomethacin (a derivative of acetic acid), non-opioid analgesics: Spazmalgin (pyrazolone in combinations) and Baralgin (pyrazolone) and antispasmodics: Drotaverine, No-shpa.
Conclusion. Thus, adequate and timely drug’s correction of premenstrual syndrome is a very urgent medical and social problem not only for the woman herself, but for the whole society as a whole. The menstrual calendars of symptoms and visual-analogue scales now very popular in Europe and allow assessing the dynamics and effectiveness of premenstrual syndrome correction. An individually selected by a gynecologist complex of medicinal and non-medicamentous measures can improve the quality of life of a modern woman [8].
Библиографическая ссылка
Карнаух Э.В., Лунина А.О. POPULAR CORRECTIVE METHODS OF PREMENSTRUAL SYMPTOMATIC COMPLEX AMONG MODERN YOUTH // European Student Scientific Journal. 2017. № 2. ;URL: https://sjes.esrae.ru/ru/article/view?id=411 (дата обращения: 05.07.2025).



